If, how, and when fMRI goes clinical
Peter Bandettini • May 18, 2018
This blog post was inspired by the twitter conversation that ensued after Chris Gorgoleski’s provocative tweet shown below. The link to the entire thread is provided here.
Before I begin, I have to emphasize that while I am an NIH employee, my opinions in this blog are completely my own based on my own admittedly fMRI-biased perspective as an fMRI scientist for the past 28 years, and not in any way associated with my employer. I don’t have any official or unofficial influence on, or representation of, NIH policies.
Why the stalled clinical implementation of fMRI?
MRI,
A current growth phase of fMRI
Just one clinical application away
How long to wait?
Potential Clinical Applications of fMRI in the Immediate Future.
- Disorder/Disease Biomarkers: Large pooled data sets that also contain structural data, genetic data, and a slew of behavioral data are just starting to be mined with advanced processing methods. Already specific networks related to behavior, lifestyle, and genetic disorders have been discovered. The long term goal here is the creation of multivariate biomarkers that can be applied to individuals either to screen, diagnose, or guide treatment with an acceptable degree of certainty. There are perhaps hard limits to fMRI sensitivity and reliability, but if the number of meaningful dimensions of information from fMRI are increased, then the hope is that this massively multivariate data may allow highly sensitive and specific individual subject and/or patient differentiation based on resting state or activation information.
- Biofeedback: It has been demonstrated that when presented in real time with useful fMRI activation-based feedback in real time on a specific aspect of their dynamic brain activity, subjects were able to alter and tune their activity. In many studies, this led to a change in an aspect of their behavior – touching on depression, phobias, and pain perception. The fMRI signal is still slow and noisy, however, of higher fidelity than other real time neuronal measures. Recently, simultaneous use of EEG has been proposed to enhance the effectiveness of real time fMRI feedback. This is still in its early stages, however, clinical trials are underway.
- Localization for Neuromodulation: An emerging area of clinical treatment is that of neuromodulation by the use of methods to stimulate or interfere with brain activity in a targeted manner either invasively or non-invasively. Deep brain stimulation, TMS, tDCS, focused ultrasound, and more are currently being developed for clinical applications – alleviating depression, Parkinson’s disease, and other disorders. The placement and targeting of these interventions is critical to their success. I see fMRI a playing a significant role in providing functional localizers so that the efficacy of these neuromodulation approaches may be fully realized.
- Assessment of locked in patients: Recent studies have shown that fMRI is superior to EEG in assessing the brain health, activity, and function of locked in patients. In some instances fMRI activity was used as a means for communication. This approach has considerable potential to be used on a regular basis in a clinical setting as no other methods compare – even in its early stages of implementation.
- Brain Metabolism/Neurovascular Coupling/Blood Oxygenation Assessment: While activation and connectivity studies dominate potential fMRI clinical applications, more fundamental physiologic information obtained using simultaneous fMRI measures with the appropriate pulse sequence, such as a combined arterial spin-labelling (ASL) for perfusion, blood oxygenation level dependent (BOLD), and/or Vascular Space Occupancy (VASO) contrast for blood volume, during a stress such as breath-hold or CO2 inhalation – or even during normal breathing variations at rest, can provide insights into baseline blood oxygenation, neurovascular coupling, and even resting and activation-induced changes in Cerebral Metabolic Rate (CMRO2). All these provide potentially unique and useful information related to vascular patency and metabolic health of brain tissue – with potentially immediate clinical applications that may fill a niche between CT angiography, ultrasound, and positron emission tomography (PET).
- Perfusion Deficit Detection using ASL: has been in existence as long as BOLD contrast and significant effort has been made to test it clinically. While the baseline perfusion information that it provides is comparable to that obtained with injected Gd contrast, its sensitivity is significantly lower, requiring a much longer acquisition time for averaging. This has slowed widespread clinical implementation.
- Perfusion Deficit Detection using resting state BOLD: This is perhaps the most promising of the possible clinical implementations of fMRI in the broadest interpretation of the name. Mapping the relative latencies of resting state BOLD fluctuations clearly reveals regions of flow deficit. This approach compares well to the clinically used approach of Gd contrast in terms of sensitivity and specificity. Creation of latency maps from BOLD fluctuations is also relatively straightforward and could be performed seamlessly and quickly in an automated manner. This approach is currently being implemented in a limited manner in hospitals in Germany and China.
- Localization of seizure foci: The flip side of mapping regions for surgeons NOT to remove for pre surgical mapping applications is the mapping of seizure generating tissue to provide surgeons with a target for removal. For certain types of seizure activity, the brain is constantly generating uniquely unusual activity, which translates into unique temporal signatures recorded with either EEG or resting state fMRI. Detection with EEG is much more easily and cheaply performed, but has less spatial precision fMRI.
- Clinical Importance of Basic Neuroscience: Many would argue that the clinical importance of basic and cognitive neuroscience research, while not having a direct clinical application, has so many secondary and tertiary influences on the state of the art of clinical practice that this is in itself a sufficient justification for continued fMRI research funding by both basic science funding agencies as well as more clinically focused agencies.
Success? How to measure it – and on what time scale?
What will it take for fMRI to be a clinical method?
Funding the vendors
Other Suggestions
Funding for fMRI is well worth it.
There are many obvious things that we humans do to a much larger degree than other animals. We construct great civilizations, we create advanced technology, we use complex language, we make art and tell stories. How do our unique capabilities guide us in figuring out how our brains are different from those of other animals, if they are?
The paper by Marek et al ( Reproducible brain-wide association studies require thousands of individuals, Nature, 602, 7902, pp 654-660, 2022 ) came out recently, and caused a bit of a stir in the field for a couple of reasons: First, the title, while an accurate description of the findings of the paper, is bold and lacking just enough qualifiers to quell immediate questions. “Does this imply that fMRI or other measures used in BWAS are lacking intrinsic sensitivity?” “Is this a general statement about all studies now and into the future?” “Is fMRI doomed to require thousands of individuals for all studies?” The answers to all these questions is “no,” as becomes clear on reading the paper.
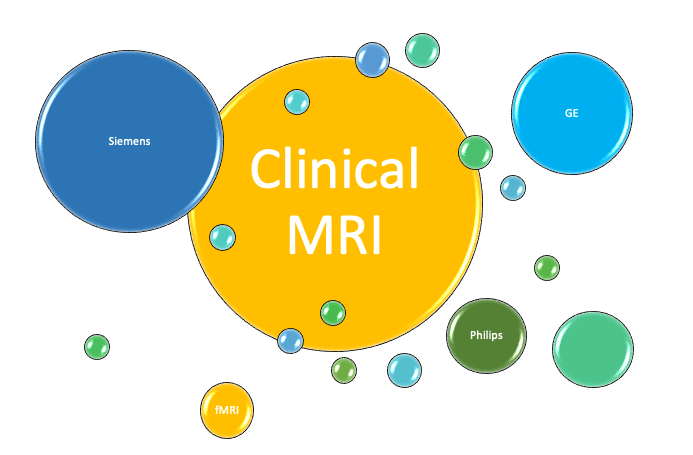
One defining and often overlooked aspect of fMRI as a field is that it is has been riding on the back of and directly benefitting from the massive clinical MRI industry. Even though fMRI has not yet hit the clinical mainstream – as there are no widely used standard clinical practices that include fMRI, it has reaped many benefits from the clinical impact of “standard” MRI. Just about every clinical scanner can be used for fMRI with minimal modification, as most vendors have rudimentary fMRI packages that are sold. Just imagine if MRI was only useful for fMRI – how much slower fMRI methods and applications would have developed and how much more expensive and less advanced MRI scanners would be. Without a thriving clinical MRI market only a few centers would be able to afford scanners that would likely be primitive compared to the technology that exists today.